bluekc nationsbenefits com Activate Card : Bluekc Provider Portal Customer Service
bluekc nationsbenefits com Activate Card : Bluekc Provider Portal Customer Service
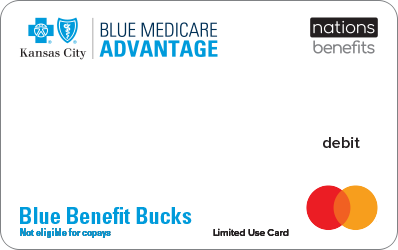
To activate your new Blue KC OTC Flex card, login into bluekc.nationsbenefits.com/activate or call 877-208-2596 (TTY: 711) and Enter the 16 digit card number and expiration date of your Benefits Mastercard® Prepaid Card.
Blue KC is a leader in the development of innovative managed care programs. Nearly one million members are enrolled in a wide range of group and individual insurance products, including health maintenance organizations (HMO), preferred provider organizations (PPO), dental, and Medicare insurance plans. Explore our website to learn more, or give us a call at 800-860-2227, Monday through Friday from 8 a.m. to 5 p.m. Central Time.
When you have Blue KC coverage that provides exclusive access to Spira Care Centers, convenience is just the beginning.
- Advanced primary care for the whole family.
- Care Guides to help coordinate care & explain benefits.
- Behavioral health consultations.
bluekc.nations benefits.com Activate Card :
Once you receive and activate your card, you can start using it online through the MyBenefits portal and the MyBenefits app and/or in person at a participating retail location near you. When at a retail location, simply swipe your card for payment.
1. Visit bluekc.nationsbenefits.com/activate or call 877-208-2596 (TTY: 711)
2. Enter the 16 digit card number and expiration date of your Benefits Mastercard® Prepaid Card.
3. Your 12-digit member ID contains 2 letters and 10 numbers
4. Enter your Date of Birth and Last Name provided to your health plan during enrollment
5. Click on Activate Card Button to activate your card.
Go mobile with the MyBlueKC app
- Take your digital ID card with you to your doctor’s visits.
- Find in-network doctors, hospitals and urgent care facilities.
- Check your claims status and see how much you may owe.
- Track your deductible and out-of-pocket spending.
Download the app* or scan the QR code:
In today’s fast-paced world of E-commerce and shifting consumer behavior, health plan members have come to expect the same expediency they experience with the largest global retailers. That’s why NationsOTC® advances consumerization of healthcare with the over-the-counter (OTC) benefit offering.
NationsOTC provides over-the-counter benefit administration services to health plans seeking an affordable, comprehensive solution in supplemental OTC services and product fulfillment. Hundreds of brand-name and generic products, health and wellness items, first-aid supplies, and a variety of foods are available across CMS-approved categories for home delivery nationwide at no additional cost.
The customizable solution also includes a modern E-commerce experience that can be tailored for your health plan.
Features of the NationsOTC Solution:-
1. CMS-compliant and fully customizable program.
2. 24/7/365 live customer service.
3. Comprehensive product formulary, including healthy foods and connectivity devices.
4. Competitive product pricing
5. Five national distribution centers
6. Nationwide 2-day delivery, at no additional cost
Member Portal
Create additional brand affinity by featuring your logo on the portal, which offers:-
- Robust search options with the ability to filter, sort and search by category, pricing, wallet, and more
- Product recommendations based on individual needs
- Expandable product detail pages complete with 360-degree images
- Benefit tracking to see available dollars to spend on plan-approved products
- Order tracking with carrier details and frequent status updates
members.nations benefits.com/aetna Activate Card
Open the Member Portal and the page will be redirect you to the member portal for profile registration. After completing registration, you will be prompted to activate your card if you have OTC Card in your hands.
Need help getting started?
If you have any questions, please call us at 877-439-2665(TTY: 711)
Member Experience Advisors are available 24 hours per day, 7 days per week, 365 days per year. Language support services are available free of charge
HOW ARE COVERAGE DECISIONS MADE?
Medical research continues to yield new technology for managing illness and disease. Blue KC determines coverage of new technology by verifying if the Blue Cross and Blue Shield Association has an existing policy. If so, Blue KC adopts that policy. If not, Blue KC researches the new technology by using scientific literature, technology reports and government agencies and by conferring with specialists in the greater Kansas City area. If there is sufficient information to demonstrate that the new technology is safe and effective, then the new technology will be considered medically necessary. Benefit coverage depends on your contract.
If there is inconclusive evidence regarding safety and efficacy, then the new technology is considered investigational. Blue KC will perform subsequent reviews to confirm any changes that may warrant coverage of the new technology.
If you are to receive a new medical test, procedure, equipment or surgery, we highly recommend calling Customer Service at the number listed on your Member ID card to determine if the specific service is covered.